
One in 13 children in the United States has a food allergy, which equates to approximately 2 in every school classroom. What’s even more shocking is the dramatic increase in food allergies over recent years: according to the Centers for Disease Control (CDC), food allergies among children increased by about 50% between 1997 and 2011.
There is no consensus as to why food allergies are on the rise. It may be a result of changes in the quality of our food—things like hybridized wheat, genetically modified soy, or pasteurized and processed dairy. It may be a result of dietary patterns—people eating the same foods day in and day out with little variation. Or it may be a result of other health conditions—things like irritable bowel syndrome (IBS) and leaky gut, which allow abnormally large food particles to be absorbed into the body.
Food allergies are a serious problem, but they are not the only type of adverse food reaction. Several different mechanisms can mediate food reactions: classic food allergies, food sensitivities, irritants, drug-like effects, and more. The range of food reactions is described next and summarized in the table below.
Classic Food Allergies
Classic food allergies occur because of an immune response to a food that is eaten. The food triggers the body to produce an antibody called IgE and a chemical called histamine. Classic allergy symptoms range from itching in the mouth or ears, runny nose, irritated eyes, sneezing, coughing, hives, skin rashes, or (in the worst case) anaphylaxis.

Anaphylaxis happens within minutes of eating a food and can be recognized by hives, swelling of the lips or tongue or throat, trouble swallowing, difficulty breathing, pale skin, vomiting, confusion, or passing out. Anaphylaxis is an emergency. If a person has an EpiPen® available, it should be administered immediately, and the person should be taken to the emergency room.
Classic food allergies are diagnosed by a skin test or blood test for IgE antibodies.
Food Sensitivities
Food sensitivities are also mediated by an immune response, but the food triggers IgG or IgA antibodies instead of IgE. These reactions do not trigger histamine but instead trigger a cascade of inflammatory chemicals. The IgG reaction is slower and can take up to 3 days to produce symptoms. Symptoms of IgG food sensitivities vary greatly from person to person, but they always relate back to inflammation. They may trigger migraine headaches or flares of chronic conditions like IBS, Crohn’s disease, eczema, asthma, constipation, or arthritis.
Because of the delayed nature of food sensitivities, a blood test to detect IgG antibodies can be helpful in identifying the offending foods. The gold standard to confirm the food reaction is to then eliminate the food until symptoms improve and then eat the food as a “challenge” to see if symptoms return.
Other Adverse Food Reactions
Enzyme deficiencies can also cause adverse food reactions. 
The most common example of this is lactose intolerance: if a person does not produce adequate amounts of the enzyme lactase, it is difficult to digest milk and other dairy products. Eating dairy then causes gas, bloating, or other digestive distress.
Some foods act as direct irritants. A good example of this is in a person who experiences heartburn. Acidic foods, such as orange juice, tomatoes, or coffee, may directly irritate the esophagus or stomach and aggravate the heartburn. Even water can be a direct irritant if it has a more acidic pH.
Some foods have drug-like effects. Food additives are the most common examples of these: monosodium glutamate (MSG) and aspartame stimulate receptors in the brain, which can lead to nerve damage as well as symptoms like appetite stimulation, migraine headaches, or foggy thinking.
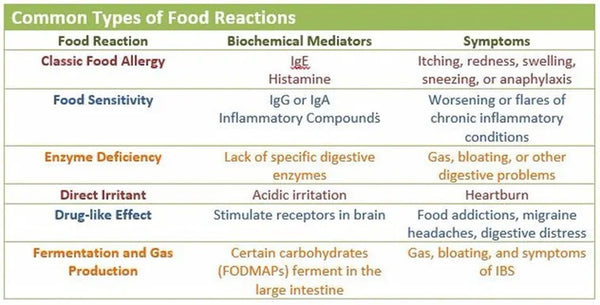
Finally, certain foods may create adverse effects because of an underlying medical condition. People who have a condition called small intestinal bacterial overgrowth (SIBO), for example, may experience an aggravation of symptoms when they eat certain carbohydrate-rich foods. This is the reasoning behind the low-FODMAP diet, which is prescribed for very specific reasons.
Making Sense of Food Reactions
Some conventional doctors may rely solely on a test for IgE food allergies to identify adverse food reactions. They may even say that other food sensitivities are not real diagnoses. I hope this article has shown you that uncovering adverse food reactions is much more complex than running one single test.
About the Author: Dr. Gerard Guillory, MD is Board Certified in Internal Medicine and has published two books on Irritable Bowel Syndrome (IBS).
